The scope of this article will review the etiology of a cavus foot, structural concerns, common signs and symptoms, gait implications, and discuss orthotic specifications that can help to minimize risk of injury and other postural concerns associated with the cavus foot. This article is available for Continuing Education Unit (CEU) credit.
The cavus foot-type is often the bane of the Pedorthic clinician, providing a challenge to provide an appropriate biomechanically-sound orthosis without too much bulk. Because of the uniqueness of this foot-type, there are a multitude of signs/symptoms as well as postural implications up the kinetic chain into the trunk. There needs to be careful consideration of proper orthotic posting and design to effectively treat foot and ankle symptoms, as well as reduce abnormal postural responses. The scope of this article will review the etiology of a cavus foot, structural concerns, common signs and symptoms, gait implications, and discuss orthotic specifications that can help to minimize risk of injury and other postural concerns associated with the cavus foot.
Pes Cavus is a Latin term meaning “hollow foot”, also called talipes cavus, cavoid foot, or simply “high-arched”. It is a multiplanar foot deformity characterized by an abnormally high medial longitudinal arch, an inverted hindfoot, an adducted forefoot, a plantar flexed 1st metatarsal, and clawing of the toes[9]. A Pes Cavus foot will typically remain “high-arched” even on weight bearing [10]. While overly pronated foot types are more common, the high arched cavus foot has the potential for significant pathological findings at the foot, lower extremity and pelvis; and it is present in about 10% of the general population[9,10].
Pes Cavus feet are commonly classified as [2,5,6,9,10]:
Neuromuscular diseases such as poliomyelitis and Charcot-Marie Tooth disease (CMT)
Congenital Conditions – such as Cerebral Palsy or Congenital Club Foot; or,
Nerve Trauma;
Idiopathic – A significant percentage of cases have no known etiology and are considered idiopathic.
Three main types of Pes Cavus have been identified:
1. Pure Pes Cavus (figure1) – This is a sagittal plane deformity, occurring either at the tarsometatarsal joint or Chopart’s joint that results in plantar flexion of the forefoot relative to the rearfoot. When the metatarsals are plantar flexed relative to the hindfoot (equinus) it creates an abnormally high arch [1]. The plantar flexed forefoot forces the hindfoot into dorsiflexion, but it also contributes to more proximal postural compensations such as knee hyperextension (recurvatum) and an increased lumbar lordosis.
2. Pes Cavovarus (figure 2) – This type is the most common type of Pes Cavus and is evidenced by a large rearfoot varus alignment, a plantar flexed 1st metatarsal, and clawing of the toes. It is most often seen in neuromuscular disorders such as CMT, but can also be idiopathic [2,4,6,11].
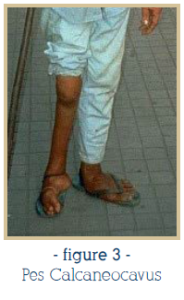
3. Pes Calcaneocavus (figure 3) – This type of pes cavus primarily occurs after paralysis of the triceps surae due to poliomyelitis [9]. The remainder of this article will relate to the typical pedorthic management of the structural components of the pes cavusfoot. The reader should keep in mind that in more extreme cases involving muscle atrophy or paralysis, as with nerve trauma or poliomyelitis, bracing above the ankle may be necessary. As pedorthists, we will at times encounter subtle to severe pes cavus patients presenting with common symptoms including lateral ankle instability, peroneal tendonitis, heel pain, sesamoiditis and lower back pain. Understanding the components of the cavus condition can help the pedorthist design the most effective orthotic device.


In a previous article we discuss that there are 6 functional foot groups (called “Quads”) that present as a child matures into their adult foot form (see Current Pedorthics May/June 2015). The cavus foot types would fall into either the “Quad C” (subtle cavus) foot type; or, the “Quad A” (severe cavus) foot group. One’s “foot type” or shape is created by the unique triplanar coupling of the hindfoot and the forefoot. In the cavus foot, potential components to consider will include degree of varus angulation of the hindfoot (rearfoot varus); presence of a forefoot equinus or valgus; and first ray (and fifth ray) positioning.
Uncompensated Rearfoot Varus (C Quad Foot Type):
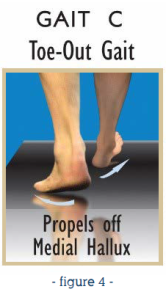
An uncompensated rearfoot varus exists when the subtalar joint (STJ) cannot pronate and therefore lacks calcaneal eversion (frontal plane deformity). The result of this excessive varus rearfoot alignment is a locked position of the midtarsal joint (MTJ), resulting in a rigid foot type with lack of natural shock attenuation. The uncompensated rearfoot varus, when coupled with a neutral forefoot alignment, is often referred to as a subtle cavus foot. These “under-pronators” have a tendency to overload the lateral column of the foot and often acquire an excessive toe-out gait from the hips in order to more easily load the medial column (figure 4). The greater the degree of heel inversion (varus), the higher the arch and the greater the extent of the out-toe gait (figure 5). This foot type may occur with or without forefoot equinus. In some cases the first ray will plantar flex in an attempt to help load the medial column of the foot but in most cases will fail to successful achieve that mission. Ultimately in gait, final propulsion will occur over the medial aspect of the 1st MTH and hallux, creating a large “pinched” callus of the great toe. Symptoms that are common to this foot type include lateral Achilles insertional tendinitis, Haglund’s deformity; as well as lower back pain, hip pain, and iliotibial band syndrome due to contracture of the lateral hip rotators.
Forefoot Valgus/Plantarflexed First Ray:
When the uncompensated rearfoot varus couples with a valgus forefoot, it is then that we begin to see the appearance of the severe cavus foot. A structural forefoot valgus is caused by a rotational malalignment of the talar head and neck (frontal plan deformity). This may be mimicked or exacerbated by the presence of a rigid plantar flexed first ray (sagittal plane deformity). There is significant force exerted on the 1st MTH at foot flat that increases throughout midstance and propulsion. Early loading of the medial forefoot has an adductory impact on the limb and results in a linear gait pattern, creating a very narrow based gait – like a tight rope walker. If the forefoot valgus / plantar flexed first ray is significant, there will be potential for severe over-supination in gait leading to potential for lateral ankle instability and heavy 1st MTH callousing. The 5th MTH will also callous due to over supination late in the gait cycle. In some cases, the 5th met will plantar flex in an attempt to stabilize the foot laterally. This can lead to lesser toe clawing and dorsal corns, as well as damaged nail beds. Other potential symptoms can include peroneus longus tendinitis, often evidenced as lateral distal shin pain just proximal to the ankle, heel pain, lateral knee pain, 5th meta-base trauma, sesamoiditis, and hypermobility of the 1st ray.
Orthotic Considerations
When thinking about the specific orthotic corrections, it is important to consider the primary components of the cavus foot type and the biomechanical implications. Orthotic correction should be primarily based on the biomechanics of the foot type and not just the symptoms.
• The ideal negative impressions are plaster non weight bearing STN slipper casts. This plaster model will give the most accurate portrayal of the FF valgus alignment relative to the heel bisection, and it will also give the most detail to the plantar flexed first ray and forefoot equinus.
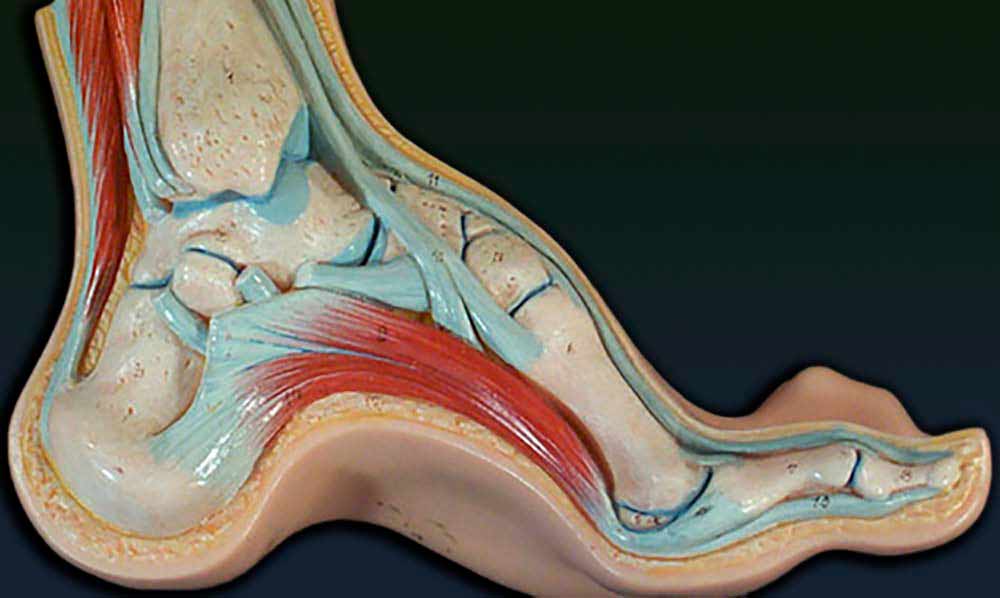
• Minimal arch fill: Many practitioners are “gun shy” as to how much to support the arch of the cavus foot. We personally find minimal arch fill is indicated. Cavus feet actually “crave” arch support the most as all of their weight is carried through the forefoot and heel, with minimal to no weight taken through the arch. Gently supporting the arch will not induce over-supination if the orthotic is posted properly, and it will provide the benefit of unloading the heel and forefoot.
• Extrinsic lateral forefoot posting will usually be necessary in more extreme cases (involving forefoot valgus) to control over-supination in propulsion.
• Channels and Cutouts: When extrinsic forefoot posting is used, consider adding a first ray channel and cutout to accommodate a rigid plantar flexed first ray if present. This will increase the effectiveness of the lateral forefoot posting and further reduce pressure on the sesamoids. A Fifth ray channel can be incorporated as well to help reduce pressure on the fifth ray when it is found to be plantar flexed.
• A high lateral heel clip and lateral border flare is helpful to keep the foot from sliding laterally off of the orthotic. The lateral heel clip may also work as a proprioceptive reminder; at contact phase, the heel will feel the lateral flange of the heel cup and will naturally want to center itself toward midline to get away from the lateral heel cup.
• Heel lifts, or shoes with elevated heels, are recommended when there is an associated forefoot equinus. This will decrease knee hyperextension and lumbar lordosis.
• Lateral Rearfoot posting? The rearfoot is typically posted at the STJ neutral position. Lateral posting of the rearfoot beyond this neutral position is typically not helpful and may actually cause injury or discomfort. The uncompensated rearfoot varus of this magnitude is often anatomically unable to evert beyond its neutral position. Any attempt to laterally post the STJ from this neutral position will usually not evert the STJ. It will apply a pronatory force to the ankle and may actually gap the medial knee joint, causing medial knee pain and potential for injury.
• Materials: Practitioners have a wide variety of material options at their disposal. Semi-rigid materials should be utilized in order to have effective control of over-supination. Soft orthotics are often prescribed, but given the rigidity of this foot and the inherent lateral instability, soft foam materials will not hold up under the heavy impact of this foot type, and the soft materials will also not provide the stability needed for lateral posting.
For on foot typing and functional gait, visit our website at: http://www.thequadrastepsystem.com/education.html or email Robertan@thequadrastepsystem.com
References:
1. Ball T, Butler M, Parsons S. Pes Cavus – Not Just A Clinical Sign. Diagnosis, Aetiology and Management. ACNR. Jan/ Feb 2013;12(6):16-19.
2. Berciano J, Gallardo E, García A, Pelayo-Negro AL, Infante J, Combarros O. New insights into the pathophysiology of pes cavus in Charcot-Marie-Tooth disease type 1A duplication. J Neurol. Sep 2011; 258(9):1594-602.
3. Burns J, Crosbie J, Ouvrier R, Hunt A. Effective orthotic therapy for the painful cavus foot: a randomized controlled trial. J Am Podiatr Med Assoc. 2006; 96(3):205-211.
4. Crosbie J, Burns J. Predicting outcomes in the orthotic management of painful, idiopathic pes cavus. Clin J Sport Med. Sep 2007;17(5):337-42.
5. Huntley JS. Optimizing the management of congenital talipes. Practitioner. Oct 2013; 257(1765):15-8,2.
6. Joo SY, Choi BO, Kim DY, Jung SJ, Cho SY, Hwang SJ. Foot deformity in Charcot Marie Tooth disease according to disease severity. Ann Rehabil Med. Aug 2011; 35(4):499-506.
7. Marks RM; Midfoot and forefoot issues cavovarus foot: Assessment and treatment issues. FootAnkle Clin. 2008 Jun;13(2):229- 41.
8. Najafi B, Barnica E, Wrobel JS, Burns J. Dynamic plantar loading index: understanding the benefit of custom foot orthoses for painful pes cavus. J Biomech. Jun 2012;45(9):1705-11.
9. Pes Cavus: Wikipedia: The Free Encyclopedia. Wikimedia Foundation, Inc. Web. 30 Sept. 2015. en.wikipedia.org/wiki/Pes Cavus.
10. Piazza S, Ricci G, Carlesi C, Volpi L, Siciliano G, Mancuso M. Pes Cavus and hereditary neuropathies: when a relationship should be suspected. J Orthop Traumatol. Dec 2010;11(4):195-201.
11. Schuberth JM, Babu-Spencer N. The impact of the first ray in the cavovarus foot. Clin Podiatr Med Surg. Jul 2009;26(3):385-93.
12. Wicart P; Cavus foot, from neonates to adolescents. Orthop Traumatol Surg Res. Nov 2012;98(7):813-28..